Reporting guidelines
This page evaluates the extent to which the journal article meets the criteria from two discrete-event simulation study reporting guidelines:
- Monks et al. (2019) - STRESS-DES: Strengthening The Reporting of Empirical Simulation Studies (Discrete-Event Simulation) (Version 1.0).
- Zhang, Lhachimi, and Rogowski (2020) - The generic reporting checklist for healthcare-related discrete event simulation studies derived from the the International Society for Pharmacoeconomics and Outcomes Research Society for Medical Decision Making (ISPOR-SDM) Modeling Good Research Practices Task Force reports.
STRESS-DES
Of the 24 items in the checklist:
- 15 were met fully (✅)
- 3 were partially met (🟡)
- 4 were not met (❌)
- 2 were not applicable (N/A)
| Item | Recommendation | Met by study? | Evidence |
|---|---|---|---|
| Objectives | |||
| 1.1 Purpose of the model | Explain the background and objectives for the model | ✅ Fully | Introduction: “Planning service delivery that separates COVID-positive patients is complicated, due to the uncertainty of the spread of SARS-CoV-2, the variability seen in symptom onset, length of infectivity, and regional delivery of dialysis. We therefore sought to support decision making in the period prior to peak infection by developing mathematical models of dialysis service delivery and patient transport. We aimed to provide reusable tools to provide rapid information under various scenarios including a worst case three month spread.” |
| 1.2 Model outputs | Define all quantitative performance measures that are reported, using equations where necessary. Specify how and when they are calculated during the model run along with how any measures of error such as confidence intervals are calculated. | ✅ Fully | Materials and methods - Outcome measures: “We estimated the the change in outpatient and inpatient workload during the epidemic in terms of COVID-positive negative and recovered, at each dialysis unit in the network. Estimates were produced over periods three to six months. We also estimated the number of patients who were required to travel to a different unit from normal and the change in travel time.”Materials and methods - Dialysis model: “The dialysis model is run 30 times to simulate 30 alternative years as, due to the randomness of infection, no two years will be exactly alike. Results show typical (median) and extreme years.” |
| 1.3 Experimentation aims | If the model has been used for experimentation, state the objectives that it was used to investigate. (A) Scenario based analysis – Provide a name and description for each scenario, providing a rationale for the choice of scenarios and ensure that item 2.3 (below) is completed. (B) Design of experiments – Provide details of the overall design of the experiments with reference to performance measures and their parameters (provide further details in data below). (C) Simulation Optimisation – (if appropriate) Provide full details of what is to be optimised, the parameters that were included and the algorithm(s) that was be used. Where possible provide a citation of the algorithm(s). |
✅ Fully | Model can technically explore multiple scenarios, but the paper presents a single scenario: worst-case three month spread. The parameters for this scenario are described and justified.Introduction: “We aimed to provide reusable tools to provide rapid information under various scenarios including a worst case three month spread.”Materials and methods - patient progression model: “The baseline model takes a worst case progression of COVID, infecting 80% of the dialysis population over 3 months.”Materials and methods - data sources: “The worst case time of spread of COVID-positive was taken from Fergeson et al. Mortality rate, time a patient was COVID-positive before admission and inpatient length of stay were local parameters.”Materials and methods - verification and validation: “We instead worked closely with clinicians, managers and informatics specialists within the local health system to review iterative versions of the model. We also opted to model a range of likely scenarios including what is widely believed to be the worst case.” |
| Logic | |||
| 2.1 Base model overview diagram | Describe the base model using appropriate diagrams and description. This could include one or more process flow, activity cycle or equivalent diagrams sufficient to describe the model to readers. Avoid complicated diagrams in the main text. The goal is to describe the breadth and depth of the model with respect to the system being studied. | ✅ Fully | Figure 1: “Schematic representation of patient pathway” (Allen et al. (2020)) 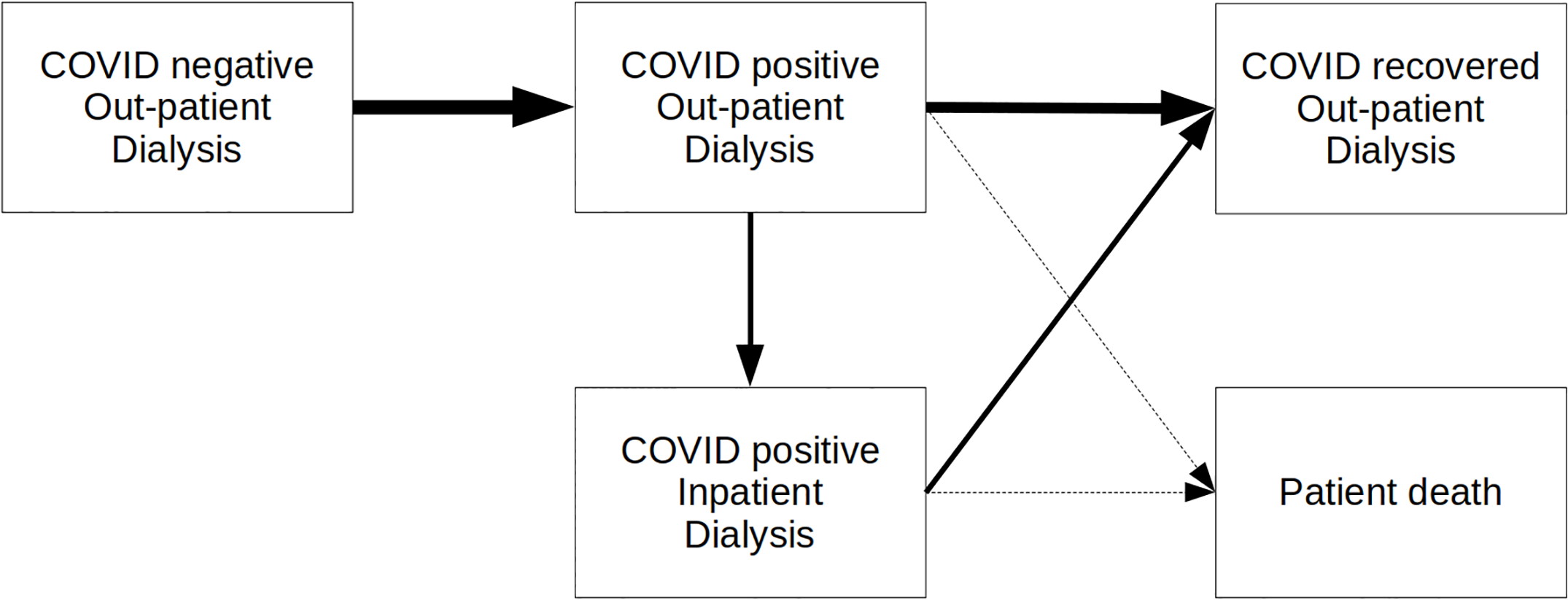 |
| 2.2 Base model logic | Give details of the base model logic. Give additional model logic details sufficient to communicate to the reader how the model works. | ✅ Fully | Materials and methods - Dialysis model section provides a detailed description of how the model works, and how patients flow through it |
| 2.3 Scenario logic | Give details of the logical difference between the base case model and scenarios (if any). This could be incorporated as text or where differences are substantial could be incorporated in the same manner as 2.2. | N/A | Not applicable (single scenario). |
| 2.4 Algorithms | Provide further detail on any algorithms in the model that (for example) mimic complex or manual processes in the real world (i.e. scheduling of arrivals/ appointments/ operations/ maintenance, operation of a conveyor system, machine breakdowns, etc.). Sufficient detail should be included (or referred to in other published work) for the algorithms to be reproducible. Pseudo-code may be used to describe an algorithm. | ✅ Fully | Materials and methods - patient progression model: “The proportions of patients and times in each phase is either fixed or sampled from stochastic distributions as given in Table 1”Table 1: Baseline model parameters (Allen et al. (2020)) 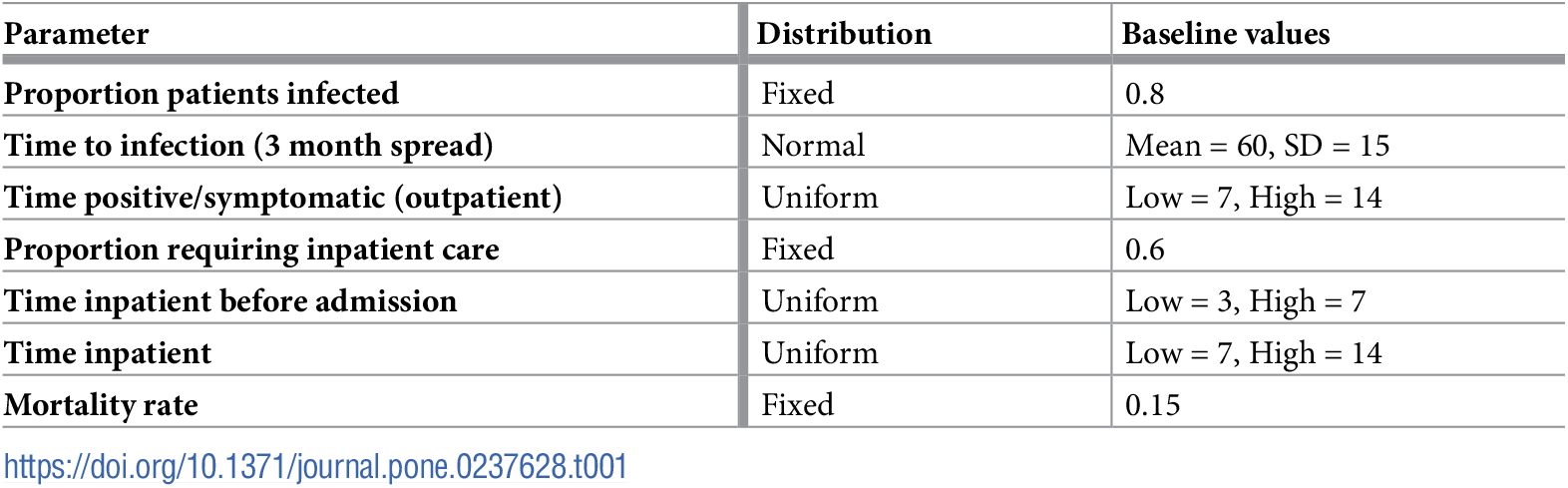 Materials and methods - unit search strategy: “When allocating patients to units, the following search strategy is employed.• COVID negative: First look for place in current unit attended. If no room there place in the closest unit (judged by estimated travel time) with available space. • COVID-positive: Place all COVID-positive patients first in Queen Alexandra Hospital, Portsmouth, and if capacity there is fully utilised open up capacity in Basingstoke. If a new COVID session is required, the model will displace all COVID negative patients in that session, and seek to re-allocate them according to the rules for allocating COVID negative patients. • COVID-positive inpatient: All inpatients are placed in Queen Alexandra Hospital, Portsmouth (though the model allows searching by travel time if another unit were to open to renal COVID-positive inpatients). • COVID-recovered: Treat as COVID negative. • Unallocated patients: If a patient cannot be allocated to any unit, the model attempts to allocate them each day.” |
| 2.5.1 Components - entities | Give details of all entities within the simulation including a description of their role in the model and a description of all their attributes. | ✅ Fully | There is one entity - patients - and these can be in different COVID states, and inpatients or outpatients.Materials and methods - dialysis model: “simulates the progression of patients through phases of COVID infection: negative, positive (with some requiring inpatient care) and recovered or died.” |
| 2.5.2 Components - activities | Describe the activities that entities engage in within the model. Provide details of entity routing into and out of the activity. | ✅ Fully | Patients are allocated to units to receive dialysis three times a week. The unit search strategy for each patient type is provided.Materials and methods - patient progression model: “all patients should receive dialysis three times weekly, with each patient allocated to a starting day for the week of either Monday or Tuesday”Materials and methods - unit search strategy: “When allocating patients to units, the following search strategy is employed.• COVID negative: First look for place in current unit attended. If no room there place in the closest unit (judged by estimated travel time) with available space. • COVID-positive: Place all COVID-positive patients first in Queen Alexandra Hospital, Portsmouth, and if capacity there is fully utilised open up capacity in Basingstoke. If a new COVID session is required, the model will displace all COVID negative patients in that session, and seek to re-allocate them according to the rules for allocating COVID negative patients. • COVID-positive inpatient: All inpatients are placed in Queen Alexandra Hospital, Portsmouth (though the model allows searching by travel time if another unit were to open to renal COVID-positive inpatients). • COVID-recovered: Treat as COVID negative. • Unallocated patients: If a patient cannot be allocated to any unit, the model attempts to allocate them each day.” |
| 2.5.3 Components - resources | List all the resources included within the model and which activities make use of them. | ✅ Fully | There are nine units, and these are the only resource, used for dialysis appointments.Materials and methods - study setting: “The service operates a network of nine centres… The Queen Alexandra will be used as the primary site for positive outpatients and inpatients with spillover to a second site (Basingstoke) when capacity is insufficient.”Supplementary Materials 1 provides further details on the units (e.g. locations, inpatient facilities, whether accept COVID-19 positive). |
| 2.5.4 Components - queues | Give details of the assumed queuing discipline used in the model (e.g. First in First Out, Last in First Out, prioritisation, etc.). Where one or more queues have a different discipline from the rest, provide a list of queues, indicating the queuing discipline used for each. If reneging, balking or jockeying occur, etc., provide details of the rules. Detail any delays or capacity constraints on the queues. | N/A | Not applicable as there are no queues |
| 2.5.5 Components - entry/exit points | Give details of the model boundaries i.e. all arrival and exit points of entities. Detail the arrival mechanism (e.g. ‘thinning’ to mimic a non-homogenous Poisson process or balking) | ❌ Not met | Not explicitly described in the paper. However, understand from Tom that it is a fixed population where patients exit the dialysis model at mortality. This is indicated by Figure 1 (Allen et al. (2020)), but as I did not feel it to be clearly detailed in the paper, this has been evaluated as not met.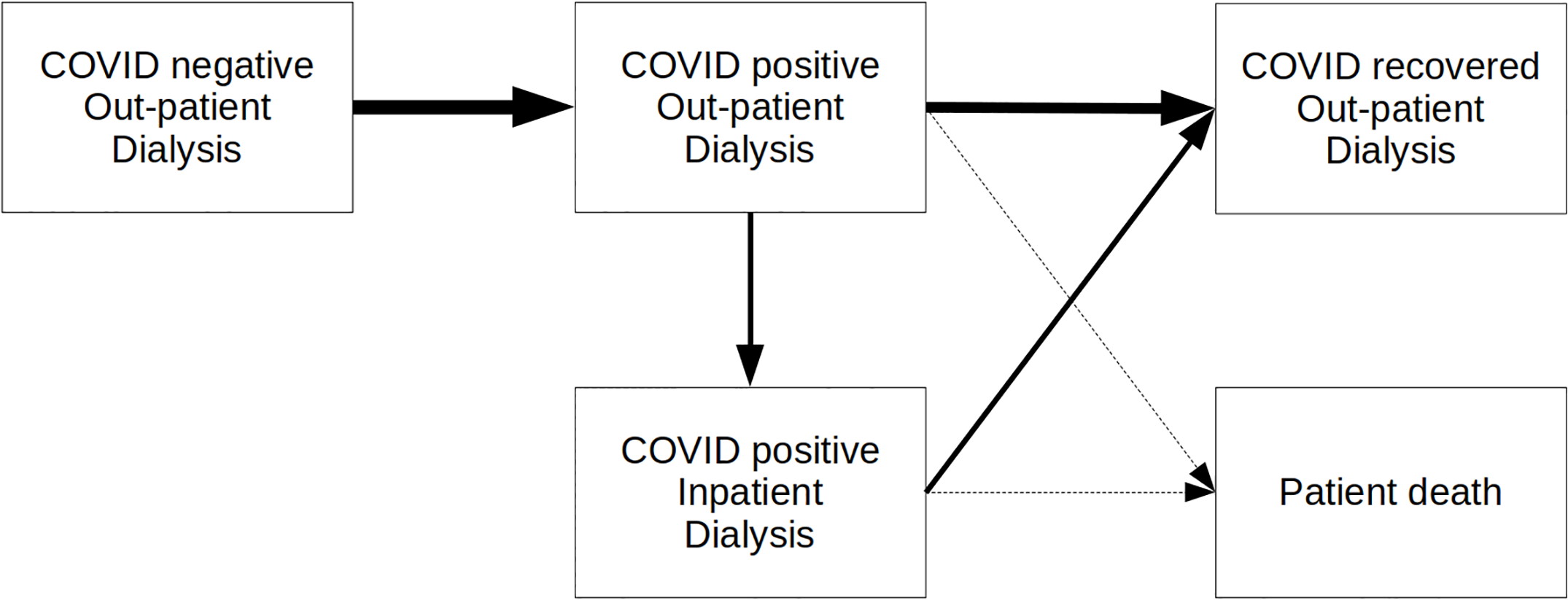 |
| Data | |||
| 3.1 Data sources | List and detail all data sources. Sources may include: • Interviews with stakeholders, • Samples of routinely collected data, • Prospectively collected samples for the purpose of the simulation study, • Public domain data published in either academic or organisational literature. Provide, where possible, the link and DOI to the data or reference to published literature. All data source descriptions should include details of the sample size, sample date ranges and use within the study. |
✅ Fully | Materials and methods - study setting: “We apply the service delivery modelling tools in the South of England in the region of Wessex: a mixed urban/rural setting where the renal dialysis service cares for 644 patients… In the analysis we excluded home patients (n = 80) and due to its separation from the mainland the Isle of Wight (n = 44).”Materials and methods - data sources: “Researchers had no access to individual patient level data. To ensure confidentiality, patient geographic locations was provided at the UK postcode sector level (alternatives might be output areas or northings and eastings). Travel times between these sectors were estimated using Routino (routino.org) with data from OpenStreetMap (openstreetmap.org). The worst case time of spread of COVID-positive was taken from Fergeson et al. Mortality rate, time a patient was COVID-positive before admission and inpatient length of stay were local parameters.” |
| 3.2 Pre-processing | Provide details of any data manipulation that has taken place before its use in the simulation, e.g. interpolation to account for missing data or the removal of outliers. | ✅ Fully | Generated travel time matrix - Materials and methods - data sources: “patient geographic locations was provided at the UK postcode sector level (alternatives might be output areas or northings and eastings). Travel times between these sectors were estimated using Routino (routino.org) with data from OpenStreetMap (openstreetmap.org).” |
| 3.3 Input parameters | List all input variables in the model. Provide a description of their use and include parameter values. For stochastic inputs provide details of any continuous, discrete or empirical distributions used along with all associated parameters. Give details of all time dependent parameters and correlation. Clearly state: • Base case data • Data use in experimentation, where different from the base case. • Where optimisation or design of experiments has been used, state the range of values that parameters can take. • Where theoretical distributions are used, state how these were selected and prioritised above other candidate distributions. |
✅ Fully | Materials and methods - patient progression model: “The proportions of patients and times in each phase is either fixed or sampled from stochastic distributions as given in Table 1… The baseline model takes a worst case progression of COVID, infecting 80% of the dialysis population over 3 months.”Table 1: Baseline model parameters (Allen et al. (2020)) 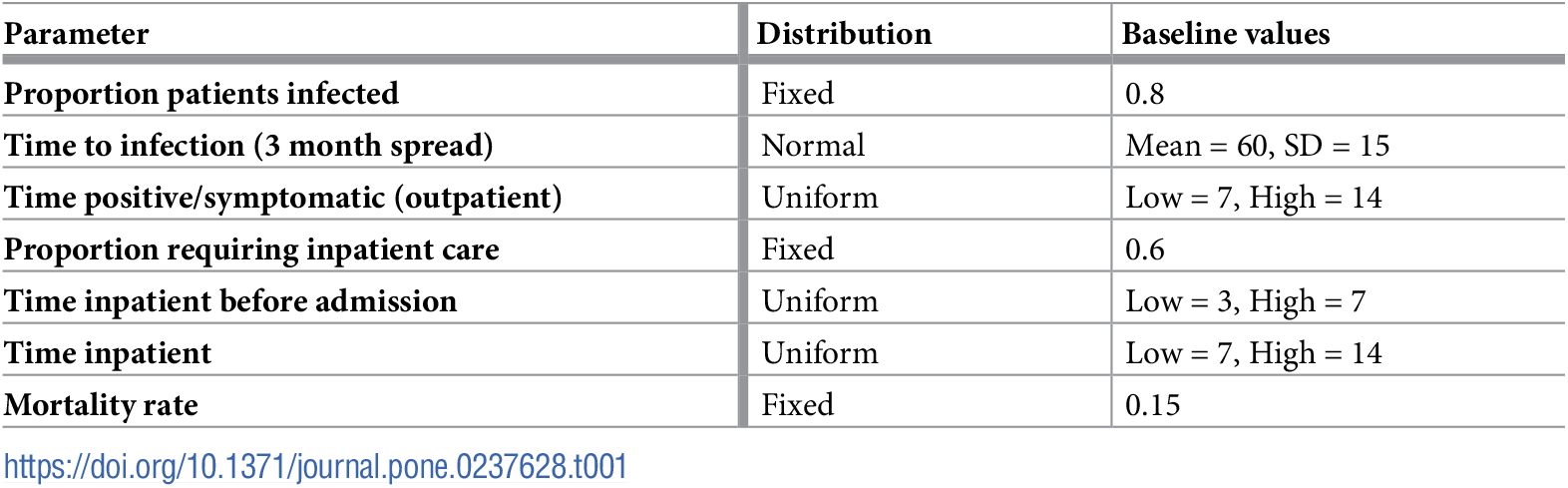 |
| 3.4 Assumptions | Where data or knowledge of the real system is unavailable what assumptions are included in the model? This might include parameter values, distributions or routing logic within the model. | ✅ Fully | Assumes worst-case scenario (80% infected in 3 months with 15% mortality).Materials and methods - patient progression model: “We assume that COVID patients must be separated from uninfected patients, and that patients who have recovered from a COVID episode do not mix with those currently testing COVID positive. We do not deal specifically with suspected COVID patients in the model, anticipating that rapid testing will soon be available to diagnose which group they belong to.”Assumes that patients travel alone - Results - dialysis network: “These patients typically require 20 minutes extra travel time to get to their temporary place of care (assuming they are travelling alone)”Discussion - limitations of the study:• “The model assumes that patients can be re-allocated to units/sessions immediately. In practice changes to session allocation (e.g. shifting from COVID-negative to COVID-positive are likely to be made a little in advance. • The results reported here assume that current capacity is maintained throughout the COVID outbreak. • We have not modelled the effect of reductions in capacity that may be caused by staff shortages. We have not modelled timing of sessions, but the model progressively allocates COVID-positive sessions as needed, and we would assume that these sessions would come later in the day, enabling cleaning at the end of the day, ready for any COVID-negative session the next morning. • We have not included home dialysis patients, which may affect inpatient demand. A likely worst-case scenario (with home dialysis patients following the transmission spread, and need for inpatient care, of the dialysis units, is that inpatient demand may be increased 15%.” |
| Experimentation | |||
| 4.1 Initialisation | Report if the system modelled is terminating or non-terminating. State if a warm-up period has been used, its length and the analysis method used to select it. For terminating systems state the stopping condition. State what if any initial model conditions have been included, e.g., pre-loaded queues and activities. Report whether initialisation of these variables is deterministic or stochastic. |
❌ Not met | Not stated - but understand from Tom that the model is non-terminating. |
| 4.2 Run length | Detail the run length of the simulation model and time units. | ✅ Fully | Daily time unit (with “per day” mentioned throughout article), and run length of three months - Materials and methods - patient progression model: “The baseline model takes a worst case progression of COVID, infecting 80% of the dialysis population over 3 months.” |
| 4.3 Estimation approach | State the method used to account for the stochasticity: For example, two common methods are multiple replications or batch means. Where multiple replications have been used, state the number of replications and for batch means, indicate the batch length and whether the batch means procedure is standard, spaced or overlapping. For both procedures provide a justification for the methods used and the number of replications/size of batches. | 🟡 Partially | Multiple replications (30). Justification for method and number of replications not provided.Materials and methods - dialysis model: “The dialysis model is run 30 times to simulate 30 alternative years as, due to the randomness of infection, no two years will be exactly alike.” |
| Implementation | |||
| 5.1 Software or programming language | State the operating system and version and build number. State the name, version and build number of commercial or open source DES software that the model is implemented in. State the name and version of general-purpose programming languages used (e.g. Python 3.5). Where frameworks and libraries have been used provide all details including version numbers. |
🟡 Partially | Materials and methods - analysis environment: “All models were written in Python 3.8. We used SimPy 3 to implement the DES model… All charts were produced with MatPlotLib… The dialysis model results were run on an Intel i9-7980XE CPU with 64GB RAM running Ubuntu 19.10 Linux.”Full details for the libraries is provided in the linked code repository within the environment file, but as this is not within the article itself (which is what STRESS evaluates), have set as partially met |
| 5.2 Random sampling | State the algorithm used to generate random samples in the software/programming language used e.g. Mersenne Twister. If common random numbers are used, state how seeds (or random number streams) are distributed among sampling processes. |
❌ Not met | Not described. From the code, can see that they did not control the random numbers using seeds or streams, and instead just used the global pseudo random number generator in Python. Hence, results vary between runs of the model. |
| 5.3 Model execution | State the event processing mechanism used e.g. three phase, event, activity, process interaction. Note that in some commercial software the event processing mechanism may not be published. In these cases authors should adhere to item 5.1 software recommendations. State all priority rules included if entities/activities compete for resources. If the model is parallel, distributed and/or use grid or cloud computing, etc., state and preferably reference the technology used. For parallel and distributed simulations the time management algorithms used. If the HLA is used then state the version of the standard, which run-time infrastructure (and version), and any supporting documents (FOMs, etc.) |
❌ Not met | Not described, but understand from Tom that as it used SimPy, it was a process-based simulation worldview. |
| 5.4 System specification | State the model run time and specification of hardware used. This is particularly important for large scale models that require substantial computing power. For parallel, distributed and/or use grid or cloud computing, etc. state the details of all systems used in the implementation (processors, network, etc.) | 🟡 Partially | Do not state model run time, but do provide hardware specification, and use parallelismMaterials and methods - analysis environment: “The dialysis model results were run on an Intel i9-7980XE CPU with 64GB RAM running Ubuntu 19.10 Linux.”Conclusion: “We have designed the tools to scale to large international dialysis planning situations and exploit parallelism and fast well known heuristics.” |
| Code access | |||
| 6.1 Computer model sharing statement | Describe how someone could obtain the model described in the paper, the simulation software and any other associated software (or hardware) needed to reproduce the results. Provide, where possible, the link and DOIs to these. | ✅ Fully | Data availability statement: “The python code and anonymous aggregate level data used this study are available from Zenodo https://zenodo.org/record/3760626. Production code is hosted on University of Exeter’s GitLab https://git.exeter.ac.uk/tmwm201/dialysis-service-delivery-covid19.” |
DES checklist derived from ISPOR-SDM
Of the 18 items in the checklist:
- 14 were met fully (✅)
- 1 was partially met (🟡)
- 1 was not met (❌)
- 2 were not applicable (N/A)
| Item | Assessed if… | Met by study? | Evidence/location |
|---|---|---|---|
| Model conceptualisation | |||
| 1 Is the focused health-related decision problem clarified? | …the decision problem under investigation was defined. DES studies included different types of decision problems, eg, those listed in previously developed taxonomies. | ✅ Fully | Planning service delivery when need to keep COVID-positive and COVID-negative patients seperate, testing the plan under worst-case scenario three-month spread.Introduction: “Rapid guidelines for dialysis service delivery have been published. These include separation of COVID-positive and COVID-negative patients; dialysis units working with transport providers to minimise the risk of cross-infection; and continuing to treat patients as close to home as possible. Planning service delivery that separates COVID-positive patients is complicated, due to the uncertainty of the spread of SARS-CoV-2, the variability seen in symptom onset, length of infectivity, and regional delivery of dialysis. We therefore sought to support decision making in the period prior to peak infection by developing mathematical models of dialysis service delivery”Materials and methods - study setting: “During the epidemic, COVID-positive patients will be treated separately from negative and recovered. The Queen Alexandra will be used as the primary site for positive outpatients and inpatients with spillover to a second site (Basingstoke) when capacity is insufficient. Patient transport services will provide COVID only ambulances with a policy of single patient transport” |
| 2 Is the modeled healthcare setting/health condition clarified? | …the physical context/scope (eg, a certain healthcare unit or a broader system) or disease spectrum simulated was described. | ✅ Fully | Patients with Chronic Kidney Disease visiting dialysis units during COVID-19Introduction: “Severe Acute Respiratory Syndrome-Corona Virus-2 (SARS-CoV-2) and the disease it causes COVID-19 (henceforth known as COVID) is causing widespread disruption to normal healthcare services, as the number COVID-positive cases increases… Although social distancing measures are in place both in the UK and internationally, patients with Chronic Kidney Disease who must visit dialysis units are limited in their ability to be fully isolated.” |
| 3 Is the model structure described? | …the model’s conceptual structure was described in the form of either graphical or text presentation. | ✅ Fully | Figure 1: “Schematic representation of patient pathway” (Allen et al. (2020)) 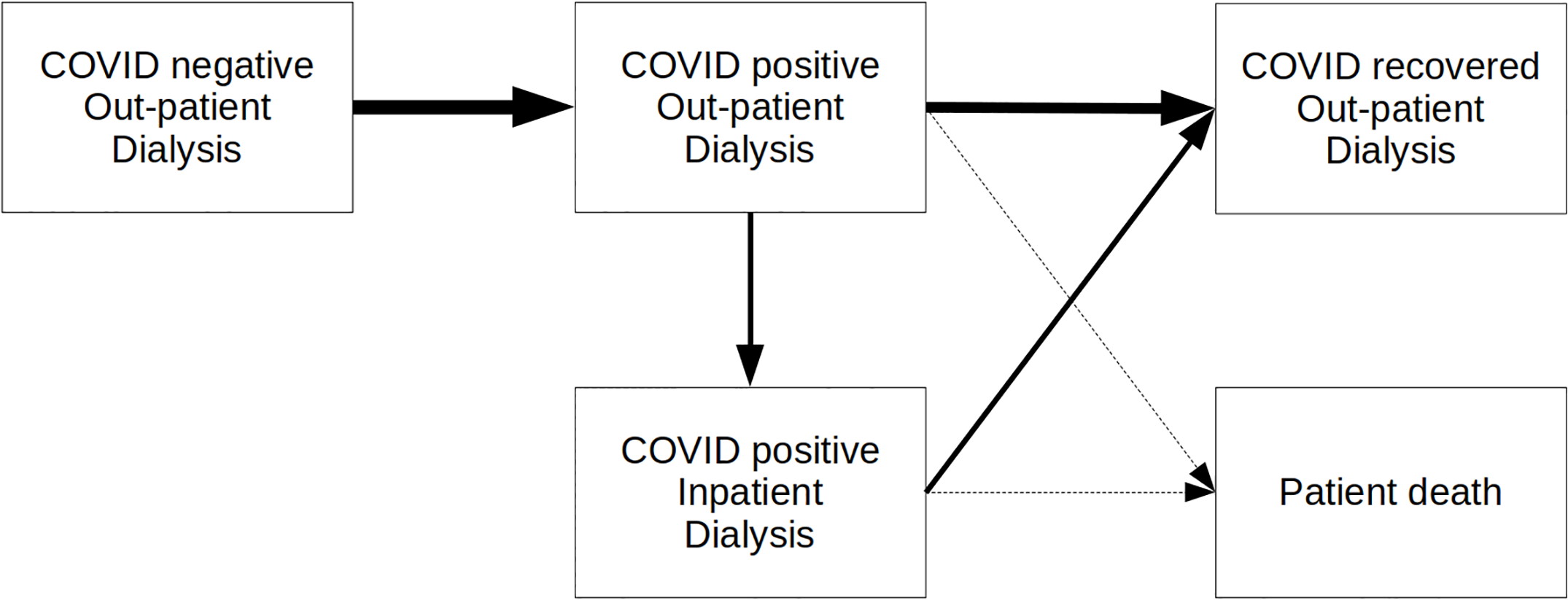 Materials and methods - Dialysis model section provides a detailed description of how the model works, and how patients flow through it |
| 4 Is the time horizon given? | …the time period covered by the simulation was reported. | ✅ Fully | Three months - Materials and methods - patient progression model: “The baseline model takes a worst case progression of COVID, infecting 80% of the dialysis population over 3 months.” |
| 5 Are all simulated strategies/scenarios specified? | …the comparators under test were described in terms of their components, corresponding variations, etc | ✅ Fully | There is a single scenario: worst-case three month spread. The parameters for this scenario are described and justified.Materials and methods - patient progression model: “The baseline model takes a worst case progression of COVID, infecting 80% of the dialysis population over 3 months.” |
| 6 Is the target population described? | …the entities simulated and their main attributes were characterized. | ✅ Fully | Materials and methods - study setting: - “We apply the service delivery modelling tools in the South of England in the region of Wessex: a mixed urban/rural setting where the renal dialysis service cares for 644 patients. The service operates a network of nine centres. The largest of which is located at the Queen Alexandra (QA) Hospital, Portsmouth. To access dialysis services 75% of patients make use of patient transport services.”Results - dialysis network: “Currently the median travel time from home to dialysis unit (one way, with a single passenger) is 14 minutes. The minimum, lower quartile, upper quartile, and maximum travel times are 1, 9, 22, and 76 minutes. Currently there is sufficient capacity for 668 dialysis patients in the outpatient sessions which are currently open, with 583 patients currently receiving dialysis (87% capacity utilisation).” |
| Paramaterisation and uncertainty assessment | |||
| 7 Are data sources informing parameter estimations provided? | …the sources of all data used to inform model inputs were reported. | ✅ Fully | Materials and methods - study setting: “We apply the service delivery modelling tools in the South of England in the region of Wessex: a mixed urban/rural setting where the renal dialysis service cares for 644 patients… In the analysis we excluded home patients (n = 80) and due to its separation from the mainland the Isle of Wight (n = 44).”Materials and methods - data sources: “Researchers had no access to individual patient level data. To ensure confidentiality, patient geographic locations was provided at the UK postcode sector level (alternatives might be output areas or northings and eastings). Travel times between these sectors were estimated using Routino (routino.org) with data from OpenStreetMap (openstreetmap.org). The worst case time of spread of COVID-positive was taken from Fergeson et al. Mortality rate, time a patient was COVID-positive before admission and inpatient length of stay were local parameters.” |
| 8 Are the parameters used to populate model frameworks specified? | …all relevant parameters fed into model frameworks were disclosed. | ✅ Fully | Materials and methods - patient progression model: “The proportions of patients and times in each phase is either fixed or sampled from stochastic distributions as given in Table 1… The baseline model takes a worst case progression of COVID, infecting 80% of the dialysis population over 3 months.”Table 1: Baseline model parameters (Allen et al. (2020)) 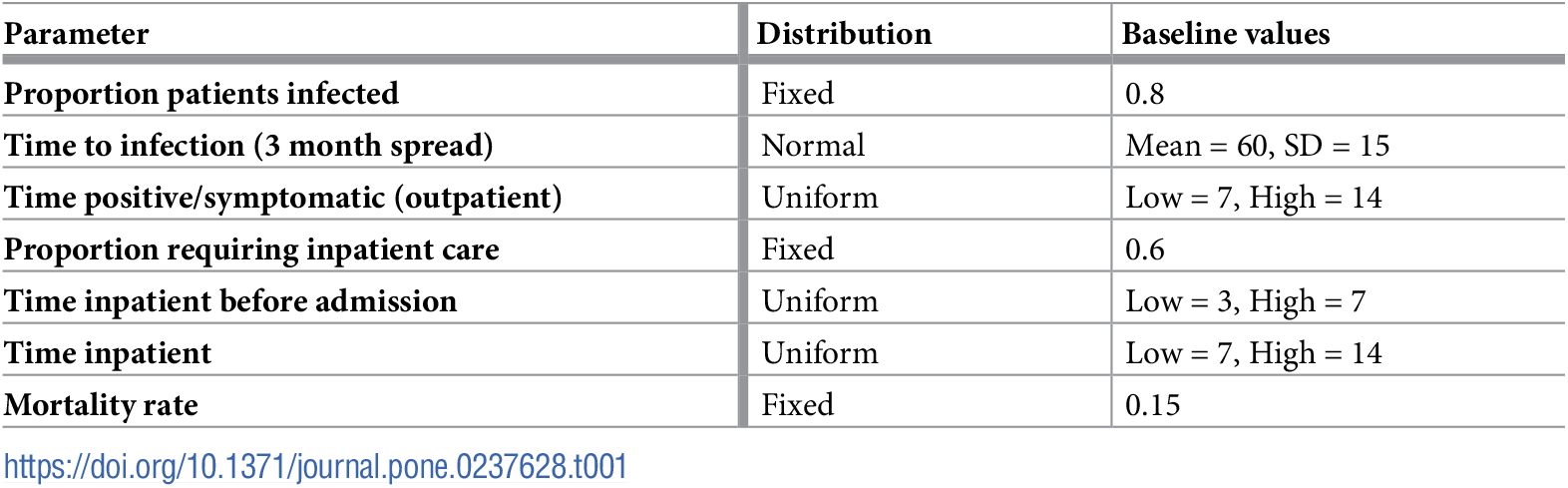 |
| 9 Are model uncertainties discussed? | …the uncertainty surrounding parameter estimations and adopted statistical methods (eg, 95% confidence intervals or possibility distributions) were reported. | ✅ Fully | All figures include the minimum and maximum from 30 trials (shown with fainter lines), alongside the median results (shown with bolder lines). Example from Figure 2 (Allen et al. (2020)): 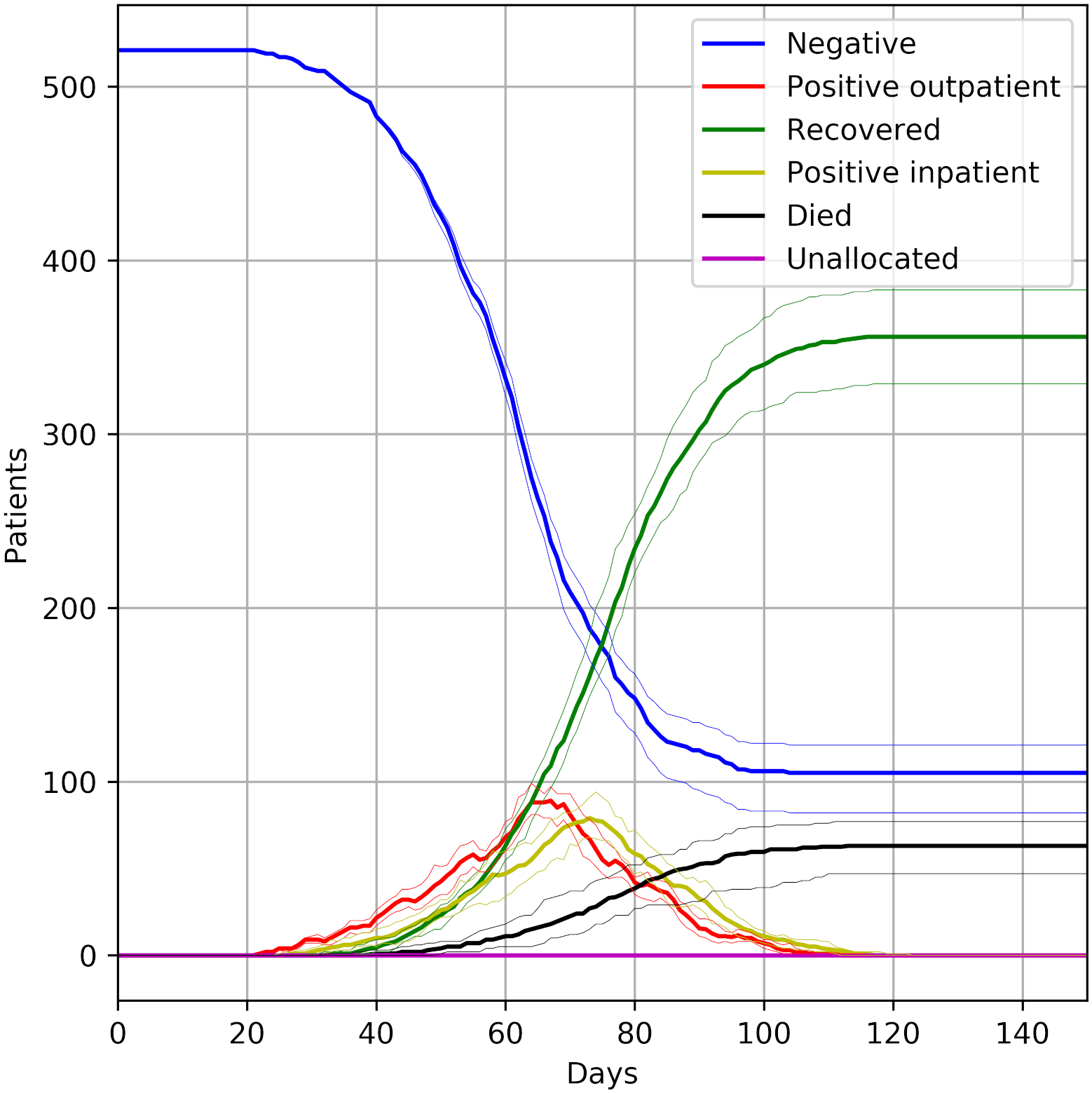 |
| 10 Are sensitivity analyses performed and reported? | …the robustness of model outputs to input uncertainties was examined, for example via deterministic (based on parameters’ plausible ranges) or probabilistic (based on a priori-defined probability distributions) sensitivity analyses, or both. | ❌ Not met | Not reported. |
| Validation | |||
| 11 Is face validity evaluated and reported? | …it was reported that the model was subjected to the examination on how well model designs correspond to the reality and intuitions. It was assumed that this type of validation should be conducted by external evaluators with no stake in the study. | ✅ Fully | Materials and methods - verification and validation: They “worked closely with clinicians, managers and informatics specialists within the local health system to review iterative versions of the model. We also opted to model a range of likely scenarios including what is widely believed to be the worst case.” |
| 12 Is cross validation performed and reported | …comparison across similar modeling studies which deal with the same decision problem was undertaken. | N/A | This was not possible as, at the point the study was conducted, similar studies on the same decision problem were not available.Materials and methods - verification and validation: “Quantitative validation of models (checking models are appropriate detailed and sufficiently accurate) is challenging in the COVID epidemic as the forecast is of unprecedented conditions” |
| 13 Is external validation performed and reported? | …the modeler(s) examined how well the model’s results match the empirical data of an actual event modeled. | N/A | This was not possible as, at the point the study was conducted, no empirical data was available.Materials and methods - verification and validation: “Quantitative validation of models (checking models are appropriate detailed and sufficiently accurate) is challenging in the COVID epidemic as the forecast is of unprecedented conditions” |
| 14 Is predictive validation performed or attempted? | …the modeler(s) examined the consistency of a model’s predictions of a future event and the actual outcomes in the future. If this was not undertaken, it was assessed whether the reasons were discussed. | ✅ Fully | Not performed but justified. Discussion - strengths of the study: “Our toolkit complements the existing epidemiological and ICU literature and aligns itself with the recent call to build new tools that can support operational decision making in health services during the pandemic. Indeed a strength of our toolkit is its practical utility in supporting the continuous safe treatment of a vulnerable group during a national or regional outbreak of COVID infection. We argue that more work like ours is needed to support health services and that the data science community must now focus on research translation. While the world’s population awaits the results of vaccine trials, the risk of a secondary wave of infections remains a reality. To protect the public and support health services under these circumstances we urgently need more research and development of novel practical decision support tools. These tools must be findable, accessible and verified. Our approach has been to make our modelling tools freely available, verifiable and open online.” |
| Generalisability and stakeholder involvement | |||
| 15 Is the model generalizability issue discussed? | …the modeler(s) discussed the potential of the resulting model for being applicable to other settings/populations (single/multiple application). | 🟡 Partially | The authors state that the tools from this work can be used in other populations - Conclusion: “The study we present applies these tools in the South of England where they were used to stress test capacity planning plans. As the pandemic progresses internationally there are risks of regional outbreaks or secondary national spikes in cases. At the start of the pandemic, there were limited operational modelling tools available to support decision makers. Our simulation toolkit is now available for use immediately by health planners. We have designed the tools to scale to large international dialysis planning situations and exploit parallelism and fast well known heuristics.”The authors provide a description of the sample in the paper, with further information on the study setting and dialysis units in the Supplementary Materials 1: Study setting geography. This supports readers understanding of potential generalisaibility.The study encourages reuse of the tools in other settings, but doesn’t explicitly describe whether the results of this study are generalisable or not, and to whom. |
| 16 Are decision makers or other stakeholders involved in modeling? | …the modeler(s) reported in which part throughout the modeling process decision makers and other stakeholders (eg, subject experts) were engaged. | ✅ Fully | Review of model - Materials and methods - verification and validation: they “worked closely with clinicians, managers and informatics specialists within the local health system to review iterative versions of the model.” |
| 17 Is the source of funding stated? | …the sponsorship of the study was indicated. | ✅ Fully | Funding: “This article presents independent research funded by the National Institute for Health Research (NIHR) Applied Research Collaboration (ARC) South West Peninsula (MA, SL). The views expressed in this publication are those of the author(s) and not necessarily those of the National Health Service, the NIHR or the Department of Health and Social Care. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.” |
| 18 Are model limitations discussed? | …limitations of the assessed model, especially limitations of interest to decision makers, were discussed. | ✅ Fully | Limitations are detailed in Discussion - limitations of the study - dialysis network model. |
References
Allen, Michael, Amir Bhanji, Jonas Willemsen, Steven Dudfield, Stuart Logan, and Thomas Monks. 2020. “A Simulation Modelling Toolkit for Organising Outpatient Dialysis Services During the COVID-19 Pandemic.” PLOS ONE 15 (8): e0237628. https://doi.org/10.1371/journal.pone.0237628.
Monks, Thomas, Christine S. M. Currie, Bhakti Stephan Onggo, Stewart Robinson, Martin Kunc, and Simon J. E. Taylor. 2019. “Strengthening the Reporting of Empirical Simulation Studies: Introducing the STRESS Guidelines.” Journal of Simulation 13 (1): 55–67. https://doi.org/10.1080/17477778.2018.1442155.
Zhang, Xiange, Stefan K. Lhachimi, and Wolf H. Rogowski. 2020. “Reporting Quality of Discrete Event Simulations in Healthcare—Results From a Generic Reporting Checklist.” Value in Health 23 (4): 506–14. https://doi.org/10.1016/j.jval.2020.01.005.