This page outlines the parts of the journal article which we will attempt to reproduce.
All images and quotes on this page are sourced from Huang et al. (2019)
Within scope
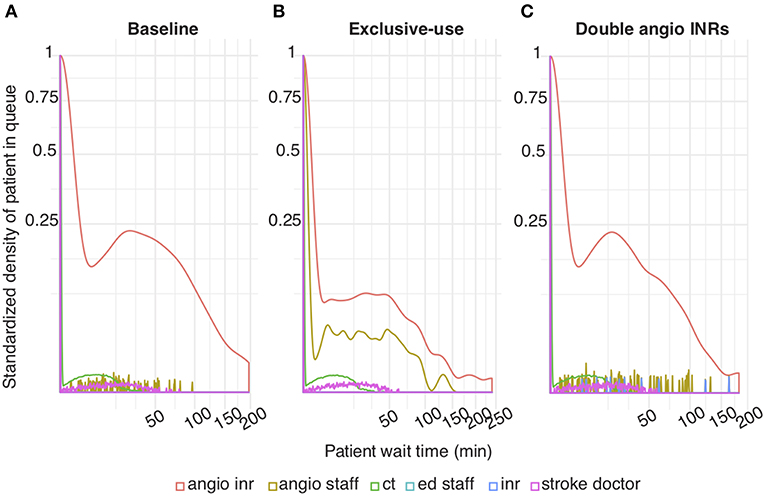
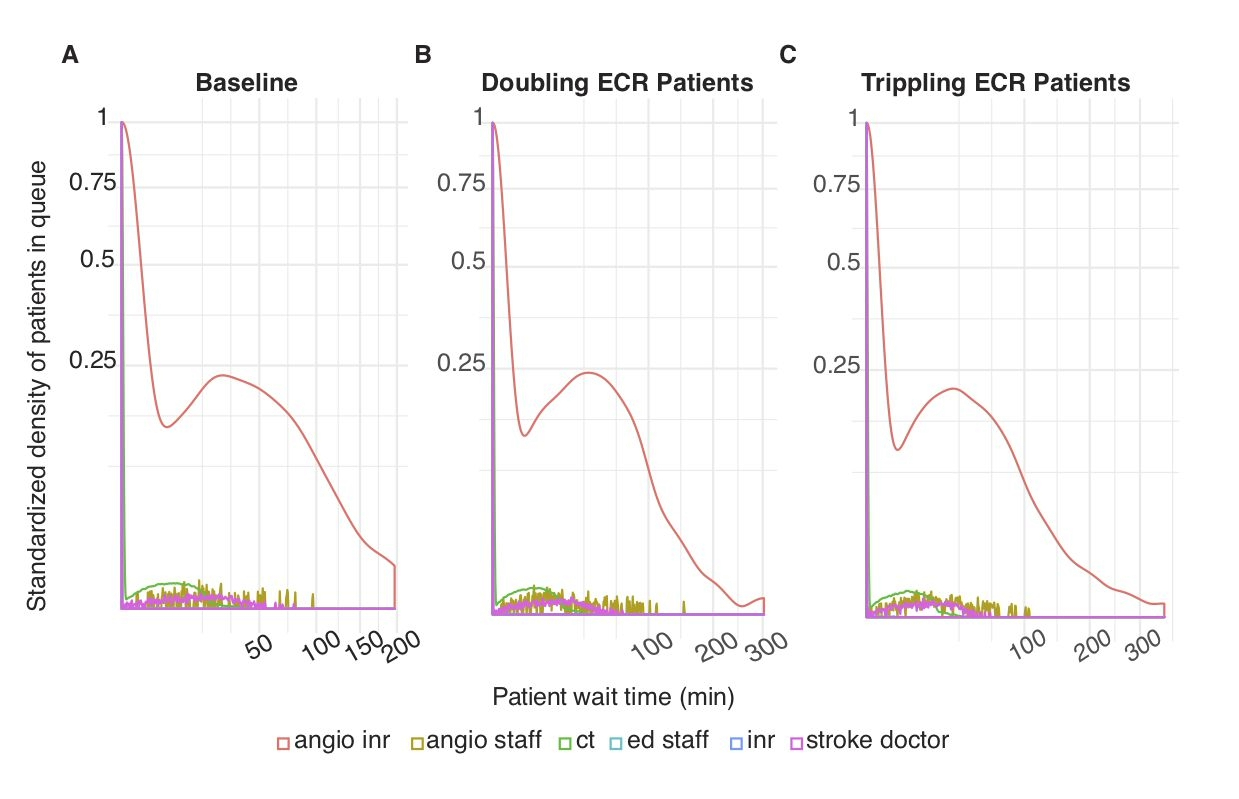
“Exclusive-Use Scenario. In this scenario, the overall wait time probability at angioINR was reduced compared to baseline (red line in Figure 2B compared to Figure 2A). This represents a decrease in ECR patient wait time for angioINR by an average of 6 min.” Huang et al. (2019)
“Two angioINRs Scenario. This scenario simulates the effect a facility upgrade to two biplane angiographic suites, but without additional staff changes. The wait time probability at angioINR was reduced compared to baseline (Figure 2C). The reduction represents an average of 4 min less in queue for angioINR.” Huang et al. (2019)
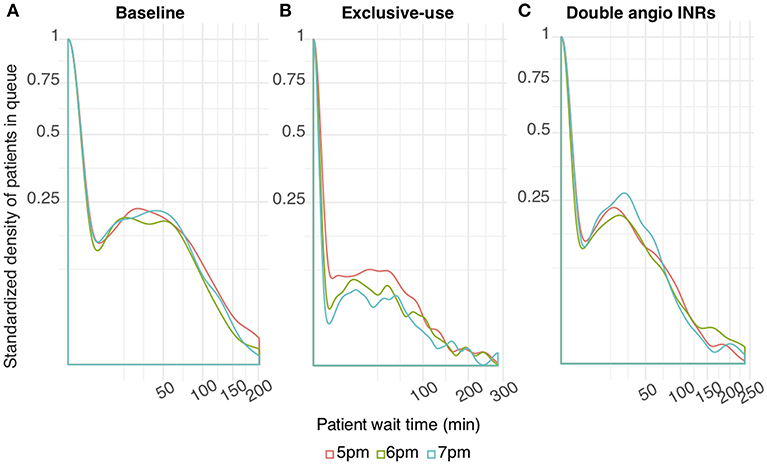
“Extended Schedule Scenario. The wait time probability at angioINR in the exclusive- use scenario was further reduced by extended work hours (Figure 3B). In contrast, work extension did not affect baseline or the 2 angioINRs scenario (Figures 3A,C). For the baseline scenario, 1 and 2 h of extra work resulted in an average wait time of 1.7 and 0.9 min reduction, respectively. For the 2 angioINRs scenario, 1 and 2 h of extra work resulted in an average wait time gain of 1 and 0.3 min, respectively.” Huang et al. (2019)
Outside scope
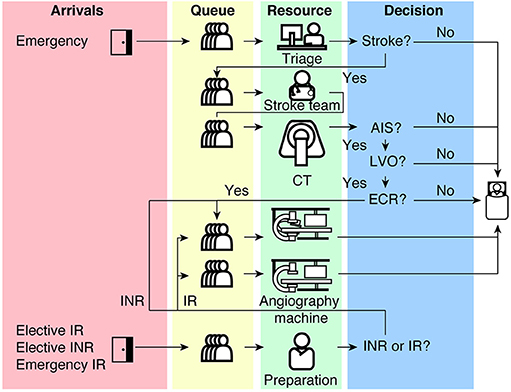
Diagram of patient flow through the model.
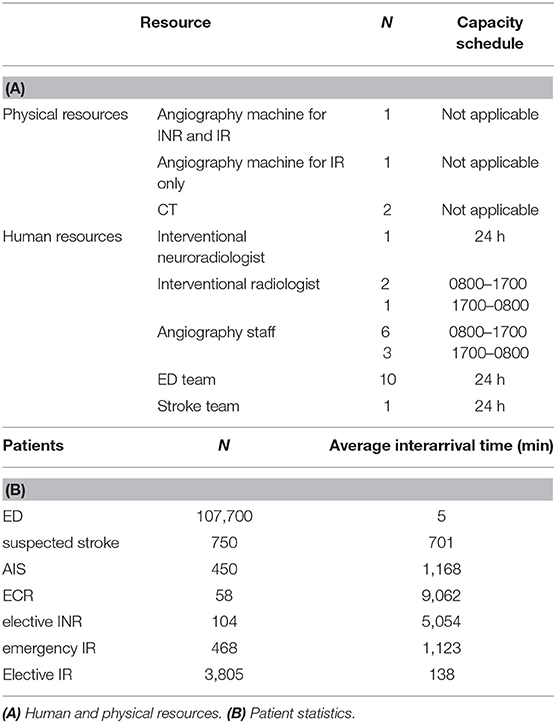
Parameters for the model.
References
Huang, Shiwei, Julian Maingard, Hong Kuan Kok, Christen D. Barras, Vincent Thijs, Ronil V. Chandra, Duncan Mark Brooks, and Hamed Asadi. 2019.
“Optimizing Resources for Endovascular Clot Retrieval for Acute Ischemic Stroke, a Discrete Event Simulation.” Frontiers in Neurology 10 (June).
https://doi.org/10.3389/fneur.2019.00653.